Deb Dana
Polyvagal Flip Chart
Understanding the Science of Safety (Norton Series on Interpersonal Neurobiology)
Vagal Components of the Parasympathetic Nervous System
The Sympathetic Nervous System
Newest Evolutionary Circuit–Ventral Vagal
Earliest Evolutionary Circuit–Dorsal Vagal
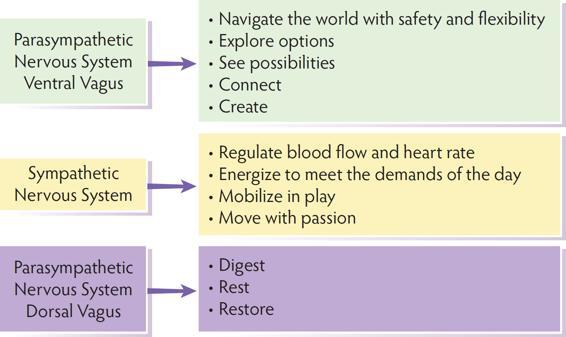
Ventral Vagal Oversees The System All Systems Online
Sympathetic Nervous System Takes Over
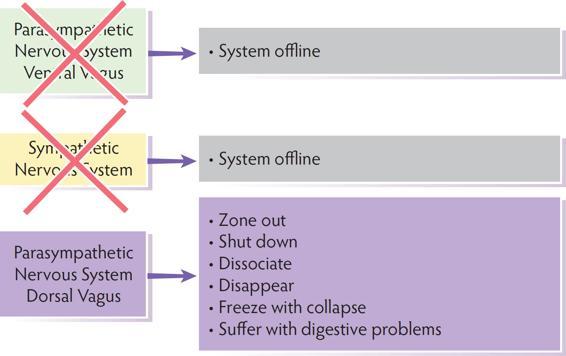
The Autonomic Impact of Trauma
Polyvagal Theory provides an updated map of the autonomic nervous system, defining how this system shapes experiences of safety and impacts the ability for connection. Polyvagal Theory gives therapists a way to bring the autonomic nervous system directly into therapy and helps clients become active operators of their own nervous systems.
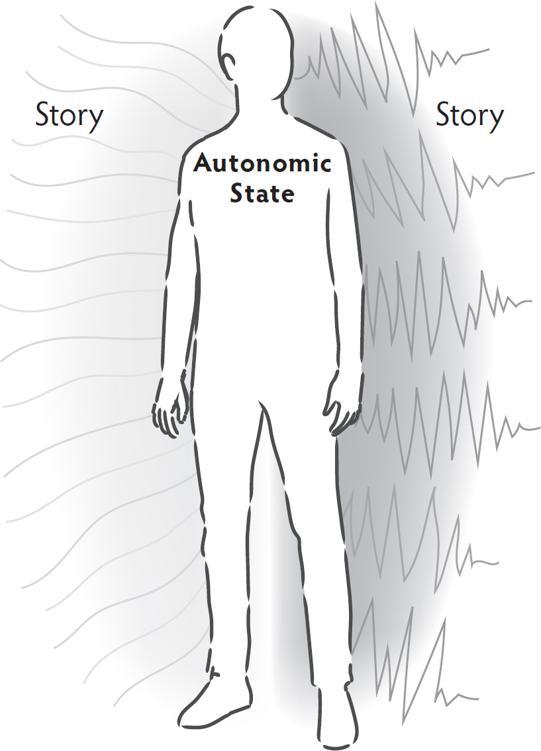
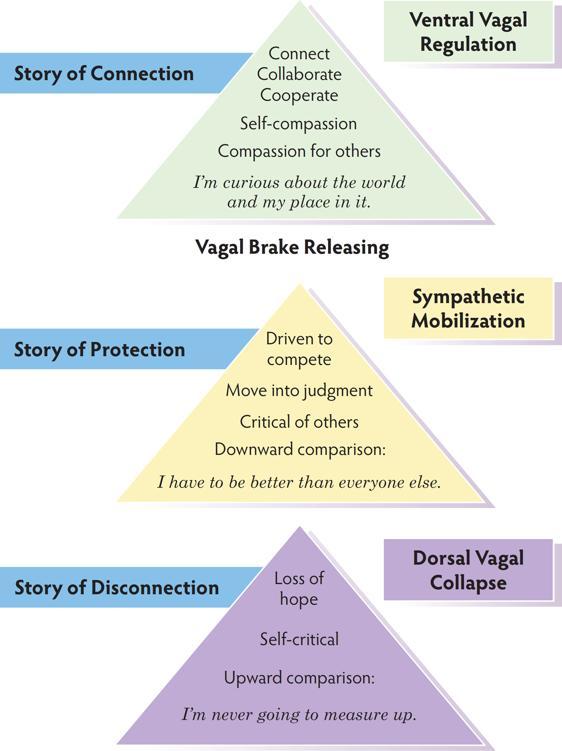
The stories clients tell themselves about who they are and how the world works begin in the autonomic nervous system. Information is sent through autonomic pathways from the body to the brain where it is translated into the beliefs that shape daily living. The brain takes the autonomic information and creates a story to make sense of what is happening in the body. If you want to change the story, start by changing the state.
Stephen W. Porges is the creator of Polyvagal Theory. Dr. Porges first outlined his theory in his Presidential Address at the annual meeting of the Society for Psychophysiological Research in 1994. His address was then published in the society’s journal, Psychophysiology (Porges, 1995). Dr. Porges has continued to elaborate and expand the theory in articles, books, and lectures. Since its introduction, Polyvagal Theory has been referenced in thousands of peer-reviewed research articles and has been incorporated into the clinical work of thousands of therapists around the world.
The Polyvagal Flip Chart is based on the constructs and principles developed and named by Dr. Porges to explain his theory. On each page of the Flip Chart, concepts related to Polyvagal Theory are presented. For those interested in reading the foundational sources, references are listed on the last page of the Flip Chart.
What is Polyvagal Theory?
Polyvagal Theory is a theory of the ways the autonomic nervous system works. Polyvagal Theory:
-
defines the ways the autonomic nervous system reacts to experiences and regulates responses
-
describes the ways the autonomic nervous system takes in information and initiates a response to help us safely navigate the ordinary demands of a day along with the extraordinary challenges we sometimes face
-
outlines a hierarchy of three biological pathways of response providing a map of the ways we predictably move in and out of engagement, mobilization, and collapse in response to daily experiences
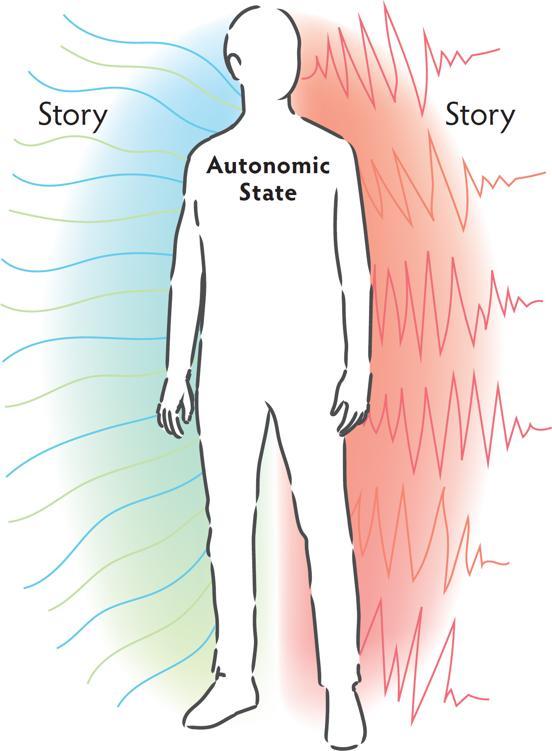
State creates story.
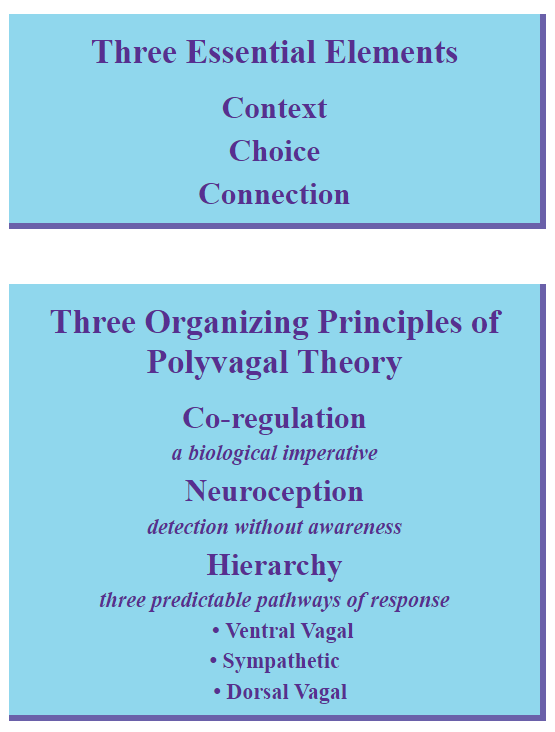
The autonomic nervous system looks for context, choice, and connection in order to find safety and regulation. When one of these is missing, a sense of unease develops and the autonomic nervous system prepares for protection. Explicitly attending to context, choice, and connection is important to the success of the therapy process.
Context—Clients don’t often ask why the therapist is doing something in a certain way and therapists don’t always think to offer that information. By providing information about why, what, and how, therapists are giving the context the autonomic nervous system needs to feel safe and engage in the therapeutic process.
Choice—When choice is restricted or when there is a feeling of being trapped, the autonomic nervous system senses danger and enacts a survival response. Where to sit, proximity, focus of the session, modality to use, and pace of work are examples of choices therapists can routinely offer.
Connection—The therapist’s ability to be in ventral vagal regulation and offer that regulating energy to clients is key to the success of therapy. Connecting with a client, tracking moments of disconnection, and returning to connection is the foundation of the therapeutic relationship. Bringing these moments into explicit awareness increases safety.
Co-regulation, Neuroception, and Hierarchy are three of the organizing principles of Polyvagal Theory.
Co-regulation is the foundation of autonomic regulation. Developmentally, co-regulation happens before self-regulation, and even after gaining self-regulating skills, there is a lifelong need for co-regulation.
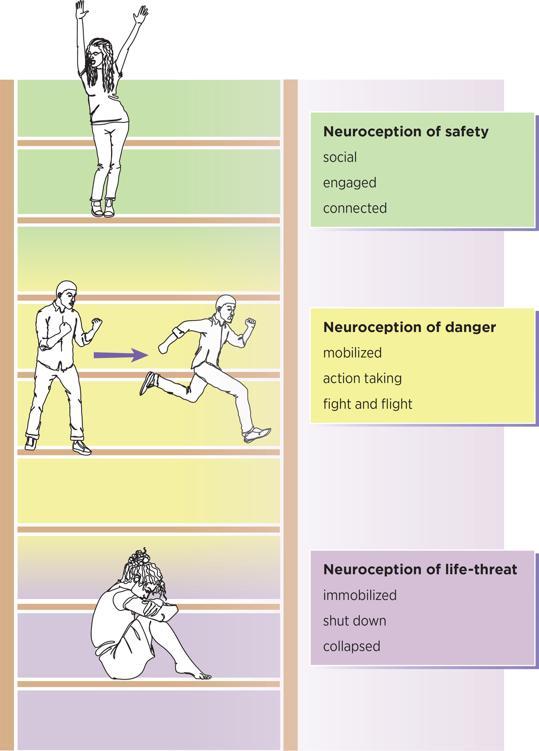
Neuroception is the word Stephen Porges created to describe the way the autonomic nervous system takes in and responds to information. Different from perception, which uses the thinking parts of the brain, neuroception is “detection without awareness.”
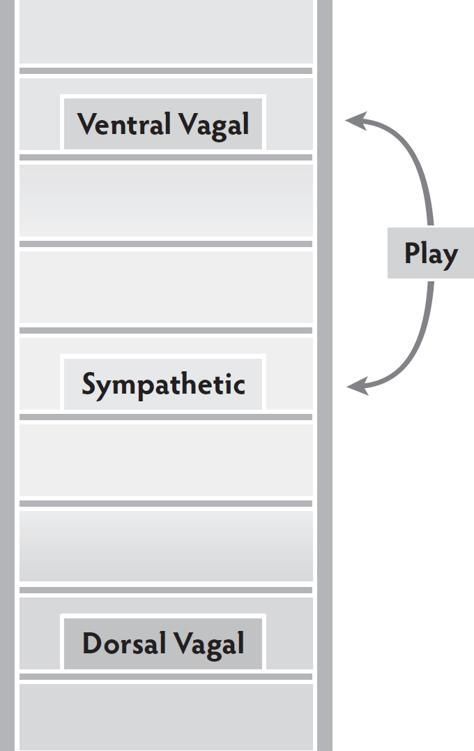
The three response states of the autonomic nervous system are organized in a hierarchy. Clients move in and out of ventral vagal, sympathetic, and dorsal vagal states in predictable ways.
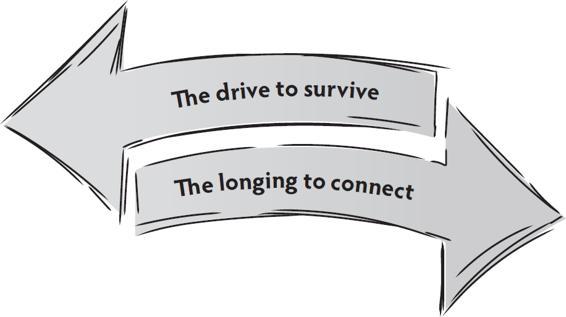
Two primary experiences coexist in the autonomic nervous system: the biological need for connection and wired-in survival responses. Sometimes these actively work together and other times they work in opposition to each other.
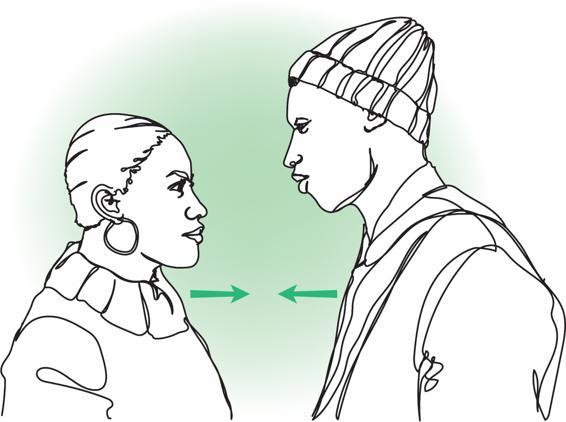
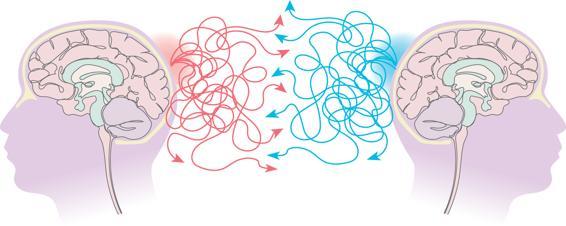
The autonomic nervous system is shaped in early relationships and continues to be shaped by ongoing experience. In the therapy session, the therapist’s and client’s autonomic nervous systems are engaged in a conversation continually broadcasting and receiving cues of safety and danger. The therapist’s ability to be regulated and offer regulation to clients is essential to the process of co-regulation.
Outside of therapy, the client’s autonomic nervous system continues to send and search for cues of safety and danger in connection with other nervous systems.
Connectedness and Co-regulation are essential constructs of Polyvagal Theory.
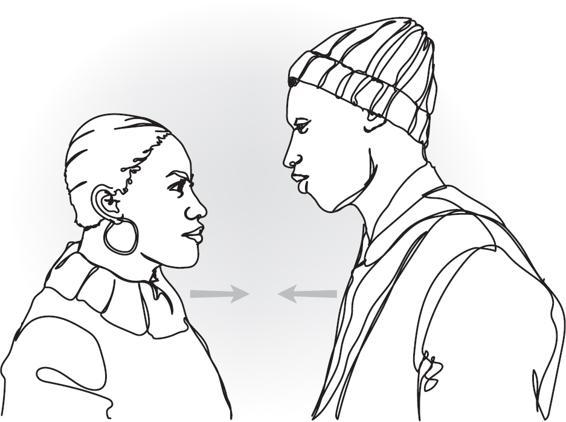
Co-Regulation
IS IT SAFE TO CONNECT?
The autonomic nervous system SENDS and SEARCHES FOR cues of safety or danger.
| Two primary experiences coexist in the autonomic nervous system. Sometimes these actively work together and other times they work in opposition to each other. | The autonomic nervous system is both shaped and regulated through interactions with others. |
| co-regulate and invite new possibilities | OR | increase reactivity and reinforce habitual survival patterns |
Neuroception the internal surveillance system, searches for cues of safety and danger inside, outside, and between. Neuroception listens to what biological systems are doing inside the body, to what is happening in the immediate environment, out into a larger environment, and to what is happening in the relationship between people—between nervous systems. Neuroception leads to changes in autonomic states, emotions, behaviors, and stories. By bringing perception to the consequences of neuroception and making the implicit autonomic experience explicit, autonomic patterns become clear; can be mapped, tracked, and ultimately shaped.
Each survival state brings important actions. When working in a regulated way, the autonomic nervous system enacts the response necessary for the present moment situation.
When the autonomic nervous system has been shaped in an unsafe environment, habitual responses that are either too much or too little are a common result. Neuroception often activates in response to something that has a familiar flavor from the past.
To bring discernment to the process of neuroception, use the question, “In this moment, in this place, with this person (people) is this response needed?”
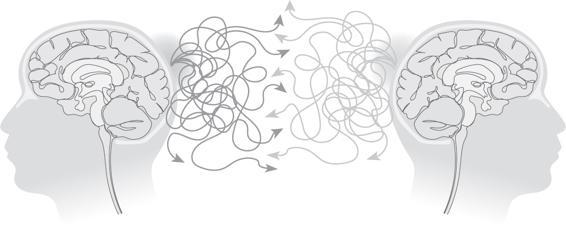
Dr. Porges created the term neuroception to describe how the autonomic nervous system takes in information about risk and safety without awareness (Porges, 2004). In his lectures he describes the process of faulty neuroception.
Neuroception
DETECTION WITHOUT AWARENESS
Neuroception describes the way the autonomic nervous system takes in information without involving the thinking parts of the brain.
Neuroception responds to cues of safety and danger inside the body, outside in the environment, and between people.
When there is a neuroceptive match:
Neuroception accurately answers the question, “In this moment, am I safe or in danger?” The autonomic nervous system moves into the state that brings the energy needed to manage the situation effectively.
When there is a neuroceptive mismatch:
| Inability to calm defense systems in safe environments leads to a habitual hypervigilant, alarmed state. | Inability to activate defense systems in a risk environment leads to an inadequate response—either dulled and unaware or high risk taking. |
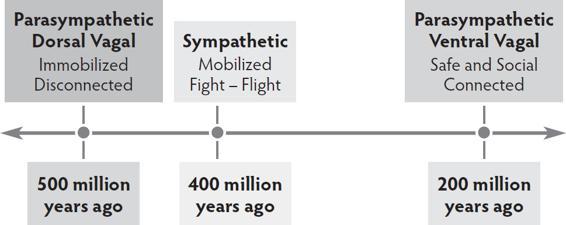
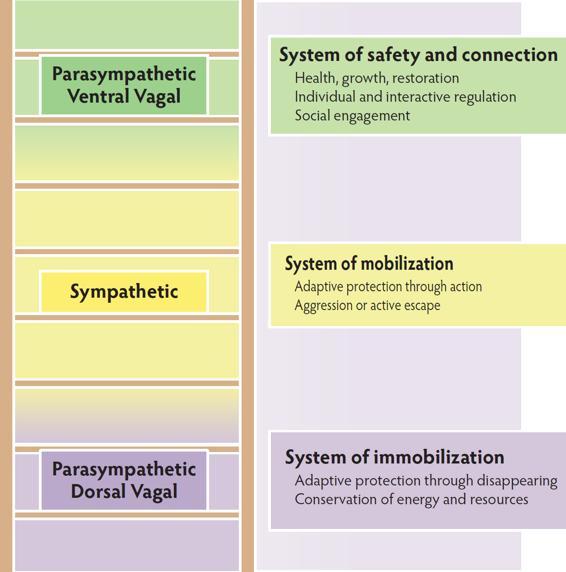
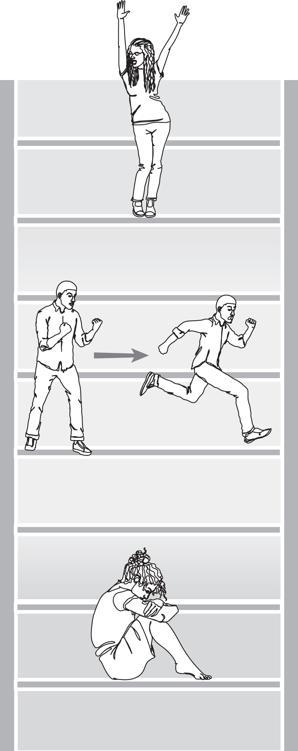
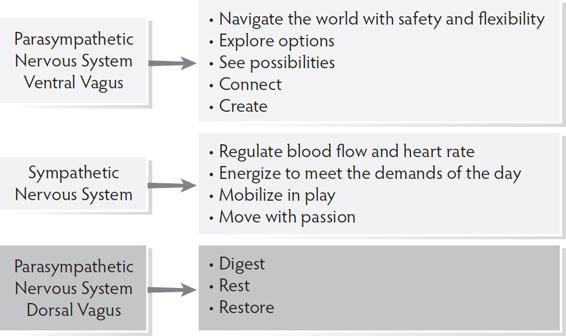
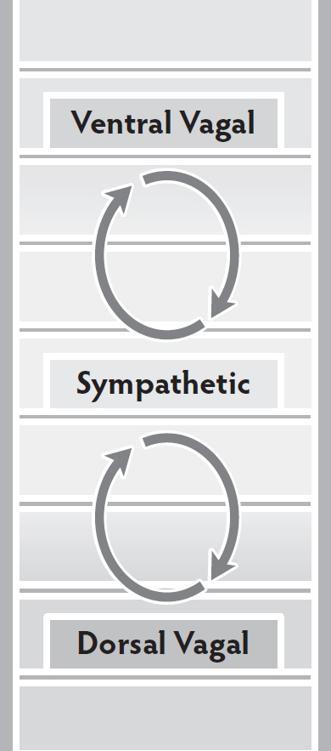
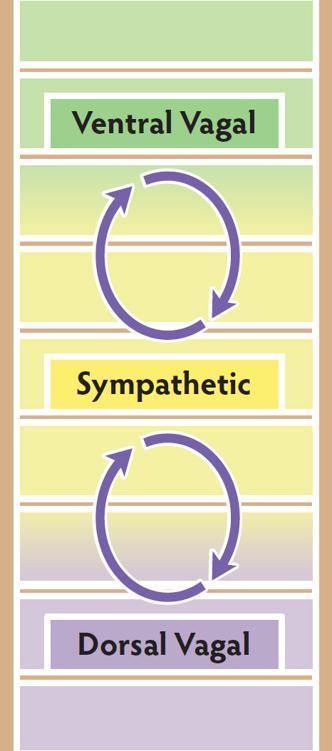
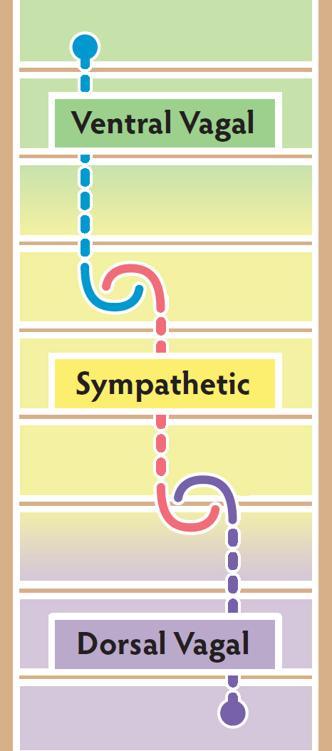
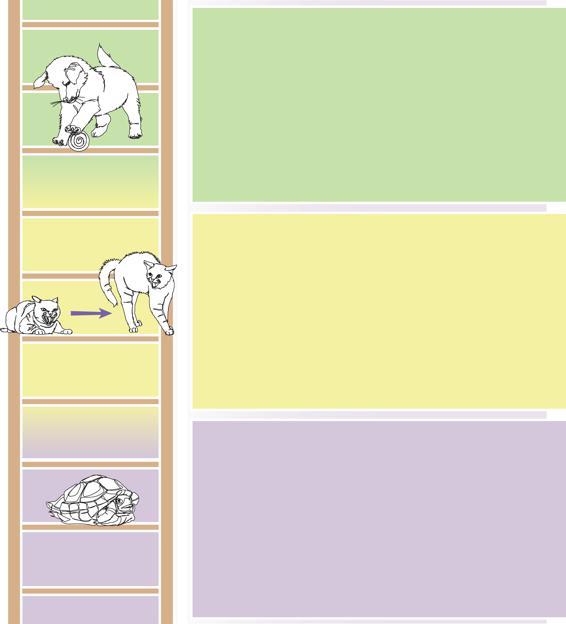
Evolution—Just like the brain, the autonomic nervous system was built over time, with newer systems added onto older ones. The earliest parasympathetic dorsal vagal state used immobilization to survive. The sympathetic nervous system developed next, adding the mobilizing strategies of fight and flight. The most recent addition, the parasympathetic ventral vagal state, brought the ability to find safety in communication and connection.
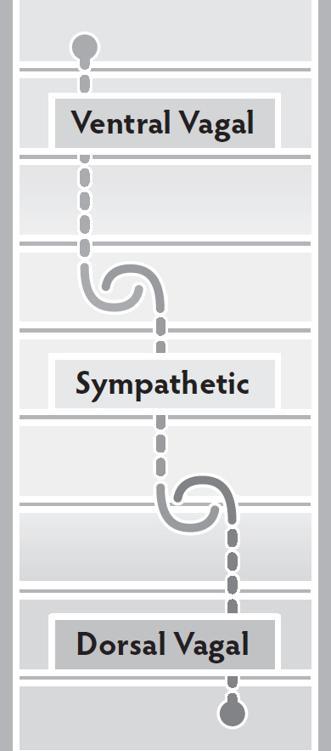
Hierarchy—The autonomic nervous system works in a predictable hierarchy.
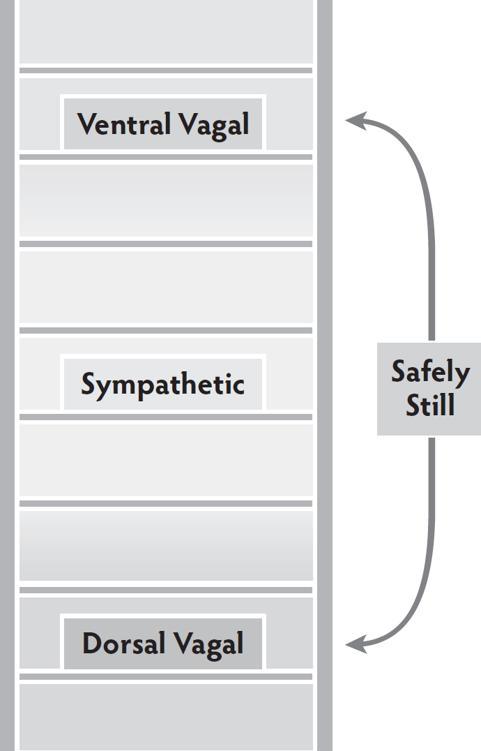
At the top of the hierarchy is ventral vagal: the state of safety and connection. When clients are confronted with a challenge that overwhelms the capacity of their ventral vagal system to maintain regulation, they move down one step into the mobilization of the sympathetic nervous system, and some form of fight or flight. And if that doesn’t resolve the challenge, the final move is to the bottom of the hierarchy—into the immobilization and disconnection of the dorsal vagal system. From the bottom of the hierarchy, to return to the state of ventral vagal regulation, clients have to safely move through some of the mobilizing energy of the sympathetic nervous system.
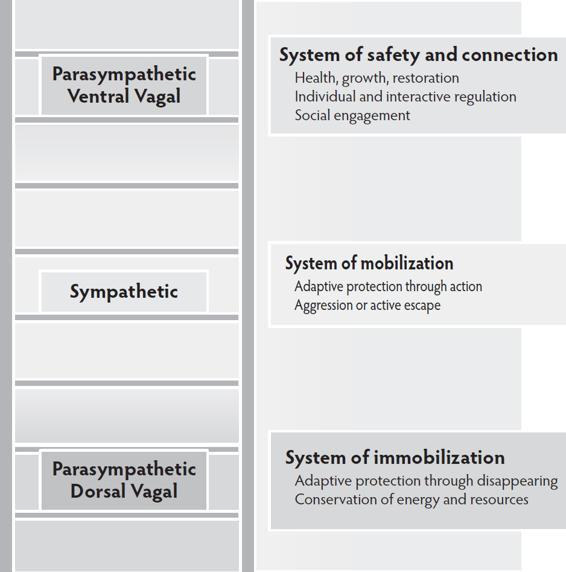
The ability to successfully adapt to the changing environment relies on the autonomic nervous system’s ability to respond and recover. Clients travel this hierarchy many times a day in small—and sometimes extreme—ways. Changes in autonomic states in response to the challenges of everyday life are a normal experience. For many clients, the move out of ventral vagal regulation leads to being stuck in a state of sympathetic or dorsal vagal dysregulation, unable to find a way back to the safety and connection of the ventral vagal state. The clinical goal is not to always be in a state of ventral vagal regulation but to be able to flexibly navigate moving down and back up the hierarchy.
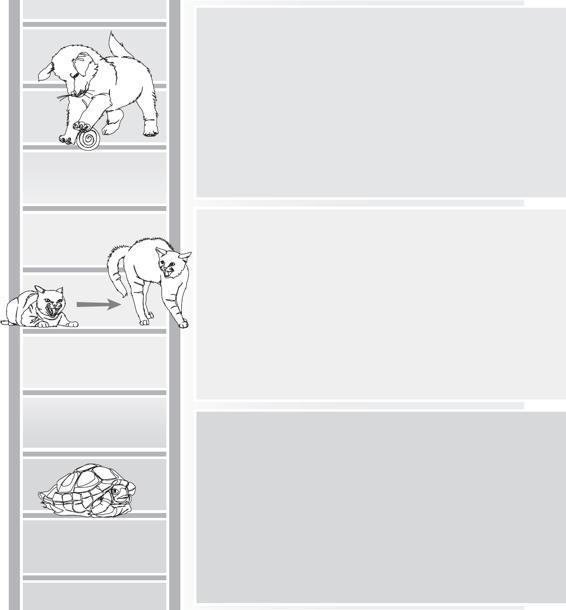
Figures depict the conceptualization of the evolutionary history of the autonomic nervous system and the autonomic hierarchy elaborated by Dr. Porges in lectures and publications on the Polyvagal Theory.
The Autonomic Timeline
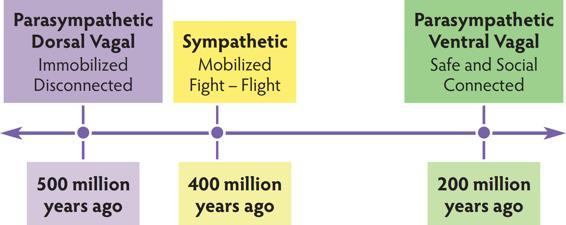
The Autonomic Hierarchy
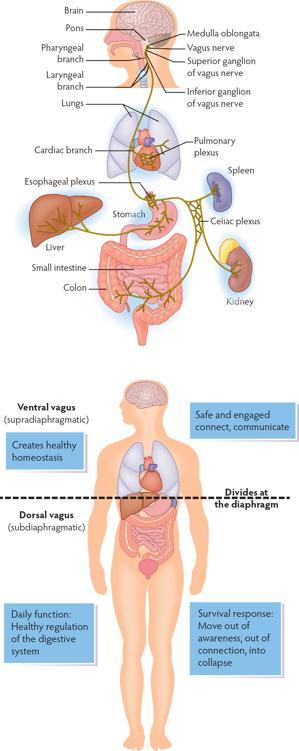
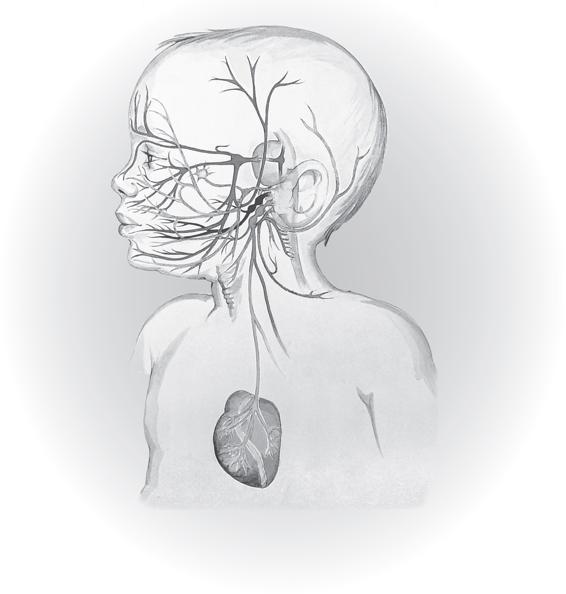
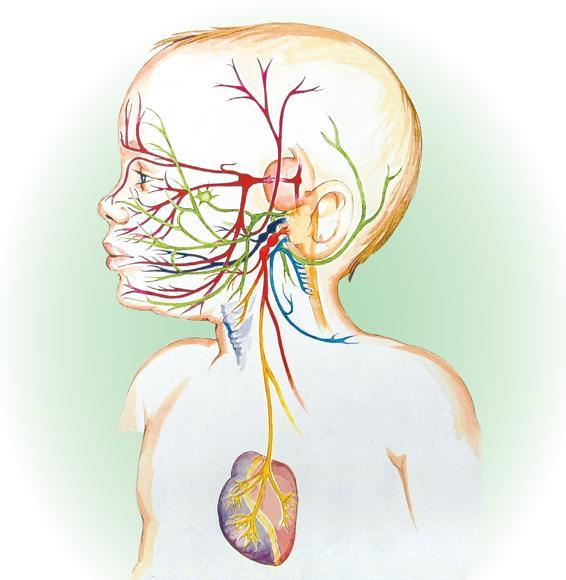
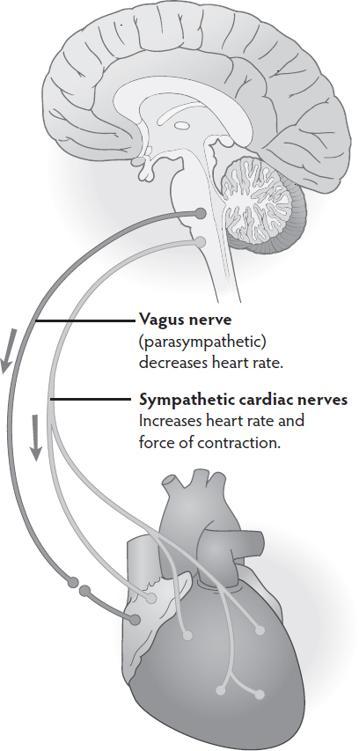
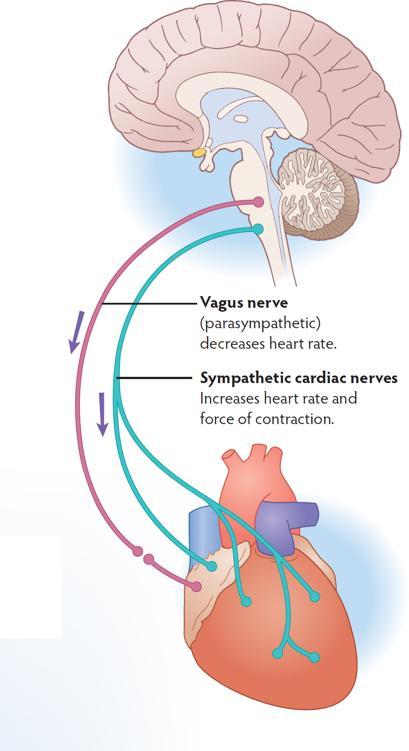
Vagus means wanderer in Latin. The vagus is the main component of the parasympathetic nervous system. The vagus is a cranial nerve (it comes from the brain and exits the skull) that begins in the brainstem and then wanders through the body, connecting with multiple organs. The vagal pathways are bidirectional, with 80% of the information traveling from the body to the brain.
The vagus is divided into two parts. From the diaphragm upward, the ventral vagus connects with the heart, lungs, pharynx, and larynx. From the diaphragm downward, the dorsal vagus connects to the stomach, liver, spleen, kidney, colon, and intestines, and is responsible for the function of the digestive system.
In daily function, the ventral vagus creates healthy homeostasis and the dorsal vagus brings healthy digestion.
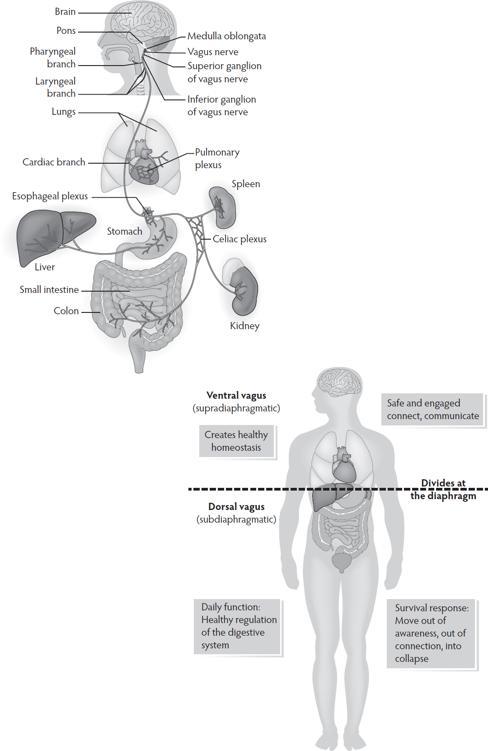
In a survival response, the dorsal vagus moves the body into conservation mode: slowing heart rate, impacting breathing, disturbing digestion, creating a sense of disconnection, numbing, collapse; a sense of going through the motions without being present.
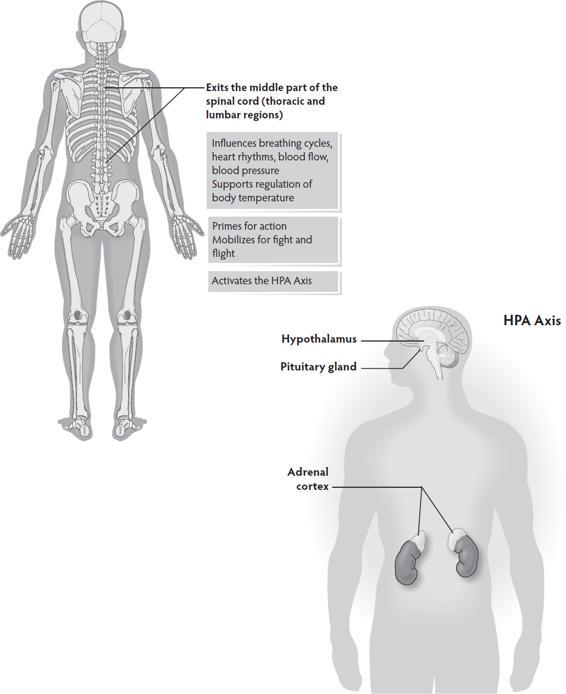
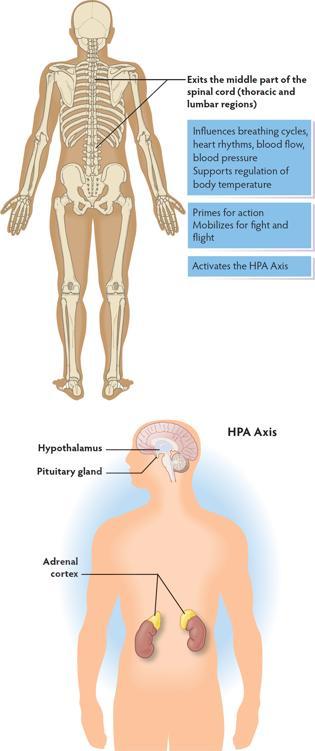
The sympathetic nervous system is a spinal nerve system (the nerves originate in the spinal cord) that helps regulate heart and breath rhythms. It works with the ventral vagal system to bring needed energy to navigate daily activities.
When triggered out of normal daily function into a survival response, the HPA axis (hypothalamus, pituary, adrenal) is activated pumping cortisol and adrenaline throughout the body.
Figures of the parasympathetic and sympathetic nervous systems are derived from Polyvagal Theory constructs. The emphases on the neuroanatomical distinction between ventral and dorsal vagal pathways and on the diaphragm are derived from Dr. Porges’s work.
Vagal Components of the Parasympathetic Nervous System
The Sympathetic Nervous System
The ability to recognize and regulate autonomic states is fundamental to the success of treatment and to safely navigating daily living. Each state has its own emergent properties. From a state of protection (sympathetic mobilization or dorsal vagal disconnection), survival is the only goal. These adaptive survival responses close the system to connection and to change. From a state of connection (ventral vagal regulation and social engagement), health, growth, and restoration are possible.
The descriptors of neuroception are elaborated by Dr. Porges in his publications and lectures.
The Autonomic Ladder
Each state has a continuum of responses.
The ventral vagus is enabled to respond when there is a neuroception of safety. The emergent properties of a ventral vagal state bring a sense of connection (to self, others, the world, and spirit), curiosity, compassion, self-compassion, and engagement.
The sympathetic state of mobilization activates from a neuroception of danger. The emergent properties of sympathetic activation bring a drive toward action in some form of fight and flight and include features of anxiety and anger.
The dorsal vagal> survival state of immobilization, shut down, and collapse comes from a neuroception of life-threat. The emergent properties of dorsal vagal bring a quality of disconnection and disappearance.
The hierarchy is a basic construct of Polyvagal Theory. In his work, Dr. Porges outlines the composition and regulatory function of the ventral vagal circuit as the newest evolutionary circuit.
Newest Evolutionary Circuit–Ventral Vagal
Safely embodied
Co-regulate
Self-regulate
Connect to self, others, the world, spirit
Acknowledge distress
Explore options
Reach out for/offer support
Resourced and resourceful

The Sympathetic Response
Mobilize to survive
Move into fight or flight
Feel out of sync with others
Driven to get needs met
Alarmed
Anxious
Hypervigilant
Misread cues
Listen for sounds of danger
Sacrifice social engagement for survival
Earliest Evolutionary Circuit–Dorsal Vagal
Withdraw
Shut down
Collapse
Become foggy, numb
Go through the motions without awareness
Disconnect from self, others, the world, spirit
Feel lost, abandoned, invisible
Disappear into a state of not knowing, not feeling, not being
The Social Engagement System is formed through the linking of Cranial Nerve X (vagus) with Cranial Nerve V (trigeminal), Cranial Nerve VII (facial), Cranial Nerve IX (glossopharyngeal), and Cranial Nerve XI (accessory).
The Social Engagement System, through the eyes, ears, voice, facial expression, and head movement both signals and searches for signs of welcome and warning. Eyes broadcast the state of the system sending signals of welcome or signs of danger. A face with expression sends clear messages. A face without expression, without movement, commonly triggers a survival response. The natural tilt to the head is a sign of safety and an invitation to connection. Tone of voice, known as prosody, emerges from an autonomic state and reveals the intention that lies beneath the words. The autonomic nervous system listens to intonation before the brain takes in information.
The construct of the social engagement system is an essential element of Polyvagal Theory, which was introduced and defined by Dr. Porges (Porges, 1998).
The image of the social engagement system in poster form is available at ppncenter.com.
The Social Engagement System
The social engagement system is our face–heart connection. The vagus (heart) and nerves in the face and head connect to control:
-
Facial expression (emotional expression)
-
Eyelids (social gaze)
-
Middle ear (hear human voice)
-
Mastication (ingestion, sucking)
-
Larynx, pharynx (vocalizing, swallowing, breathing)
-
Head turn and tilt (social gesture, orienting)
Through these pathways you send and search for signs of welcome and signals of warning.
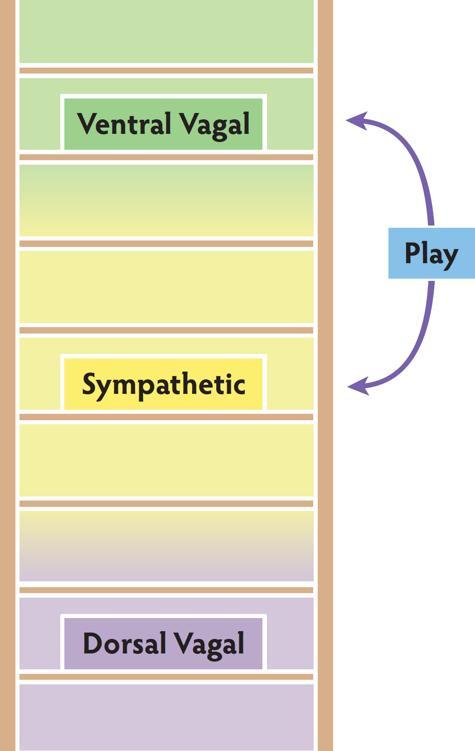
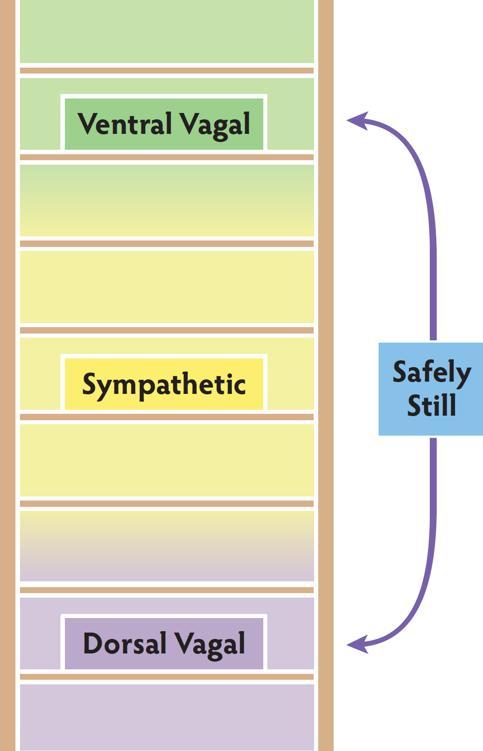
The ventral vagal and sympathetic systems work together to activate the state of play. Play exercises the vagal brake and strengthens the ability to move between activity and calm. If sympathetic mobilization overwhelms the capacity of the vagal brake, the excitement of play quickly turns from fun to fear. Play uses the Social Engagement System to regulate mobilization.
Stillness is a complicated autonomic activity. The challenge is to become still without being pulled into shut down. To become safely still, the dorsal pathway brings immobilization and the ventral pathway adds the sense of connection. These two circuits work together to support experiences of intimacy and social behaviors that require stillness.
In his lectures Dr. Porges describes the properties of hybrid states (e.g., play, freeze, intimacy).
Blended States
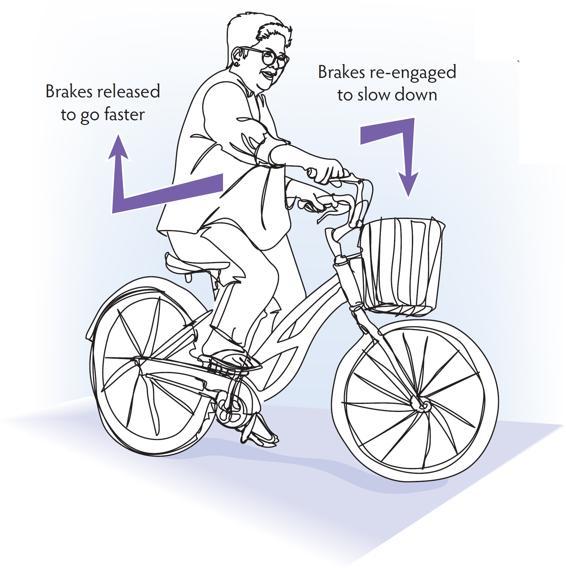
The purple pathway in the image is a ventral vagal circuit going to the heart’s pacemaker (the sinoatrial node of the heart). Its job is to slow resting heart rate to between 60–80 bpm and to regulate how much sympathetic energy (coming through sympathetic cardiac nerves represented by the green pathway) is available in the system moment to moment. Because of this regulating action, this vagal pathway is known as the vagal brake.
Using image and movement helps to understand the vagal brake and feel the rise and fall of energy and activation. Besides the brakes on a bicycle, other commonly used images include opening and closing a door or a window; using a dimmer switch or volume control; raising and lowering a bridge. With an image or movement, clients can practice using their vagal brake to increase energy and meet a challenge from the safety of the ventral vagal state.
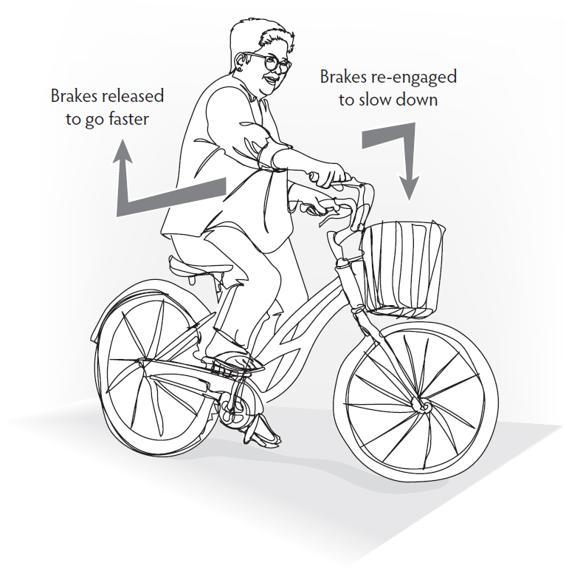
In the development of Polyvagal Theory, Dr. Porges introduced the construct of the vagal brake and outlined its features (Porges, 1996).
The Vagal Brake
-
efficiently increases and decreases heart rate
-
brings mobilization without a move into a sympathetic fight and flight survival response
-
supports the ability to move between action and calm
The ventral vagal system holds the sympathetic and dorsal vagal systems in its influence. When the ventral vagal system is active, the other two systems are able to work in the background doing their nonreactive, everyday jobs, and clients are able to effectively engage with the world.
When the vagal brake is unable to hold and the system moves into sympathetic mobilization, the emergent properties of the ventral vagal state are no longer accessible. When a client moves out of ventral into sympathetic, biology restricts options for response, activates fight and flight, and takes away capacity for social engagement.
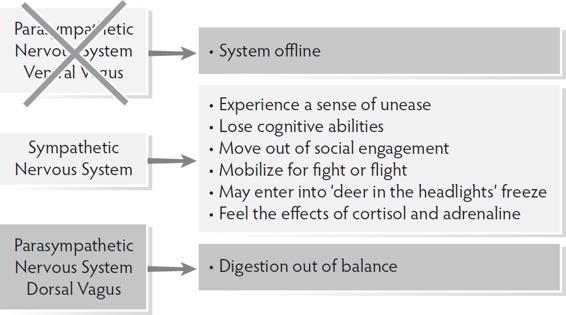
When mobilization of the sympathetic system doesn’t resolve the challenge, the autonomic response is a move into dorsal vagal shut down. In this state, biology brings disconnection from self, others, and the environment and a move out of the present moment.
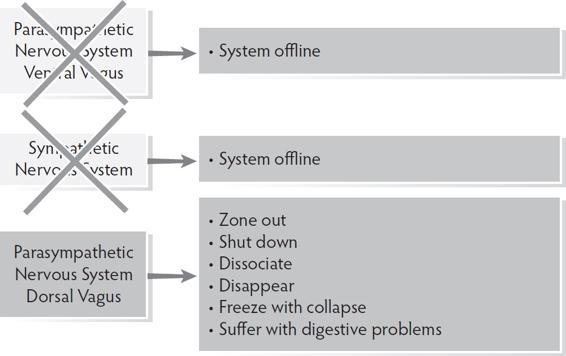
Polyvagal Theory defines the hierarchical movement between states. Dr. Porges further elaborated the concept of the ventral vagal state overseeing and coordinating the components of the autonomic nervous system (Porges, 2017).
Ventral Vagal Oversees The System All Systems Online
Sympathetic Nervous System Takes Over
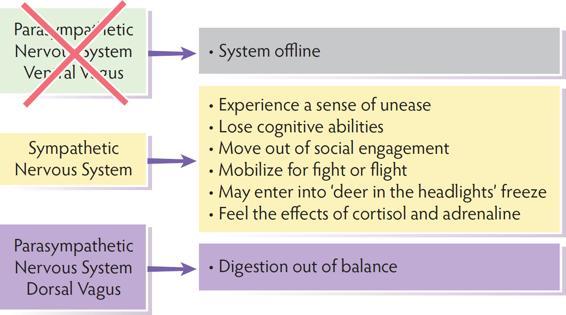
Dorsal Vagal System in Charge
Trauma impacts the autonomic nervous system both in acts of commission (things done to a person) and acts of omission (neglect, unpredictable connection). Since connection is a biological imperative, chronic disconnection is traumatic.
When opportunities for co-regulation are intermittent or dangerous, clients don’t learn the skill of co-regulation and have to depend on self-regulation. Then, instead of emerging from the safety of the ventral vagal state, self-regulation is based in the survival response of a sympathetic or dorsal vagal state.
When the autonomic nervous system has been shaped by trauma, client response patterns are biased toward protection and survival rather than connection and social engagement.
There are two common autonomic response patterns seen in clients.
Some clients live with a habitual sympathetic activation and are unfamiliar with the ventral vagal state. Entering into ventral vagal regulation can bring a flavor of danger.
To build the capacity to safely stay in ventral vagal regulation, explicitly recognize micro-moments of ventral vagal regulation when they happen and bring co-regulation to the experience. Notice when you and your client are sharing a moment of ventral vagal safety and connection and name the experience.
Clients who live with a habitual dorsal vagal immobilization often find the beginning move upwards out of shutdown into some mobilizing energy to be frightening, precipitating a return to collapse. With these clients, work with a titrated experience of activation and use co-regulation to provide the needed connection to safely continue the move through mobilization into regulation.
Resilience is an outcome of being able to flexibly navigate the autonomic hierarchy. It is a normal, everyday experience to move down and up the autonomic ladder many times a day. Suffering happens when we are pulled into a survival response and get stuck there. Well-being comes from recognizing moments of dysregulation and connecting with resources to return to regulation.
The ways trauma retunes the nervous system is described by Dr. Porges in his publications and lectures (Porges, 2017).
The Autonomic Impact of Trauma
Co-regulation is often unavailable, unpredictable, and unsafe.
Self-regulation may be inadequate and unsuccessful.
Opportunities to build autonomic circuits of connection are interrupted.
Adaptive survival responses override social engagement.
Patterns of protection replace patterns of connection.
Stuck in an Autonomic Cycle
The ventral vagal state of safety and connection feels unfamiliar, unsafe, and is unsustainable, leading to an ongoing cycle of sympathetic mobilization, brief ventral regulation, return to sympathetic mobilization.
There are not enough resources (internal abilities, environmental safety, social support) to safely engage with sympathetic mobilizing energy, creating a cycle of disconnect—activated distress—disconnect.
Navigating the Autonomic Hierarchy with Flexibility
Anchored in ventral with an active vagal brake Move between ventral and sympathetic with ease
Triggered into sympathetic mobilization
Utilize resources to safely discharge energy and return to a ventral state of regulation
Pulled into shut down
Create a small moment of mobilization
Use the energy of sympathetic in an organized way and continue to move through sympathetic into the ventral state of safety
We make sense of the world by making comparisons. It is a normal part of daily experience and helps us place ourselves in relation to others. There are two common pathways of responding to the comparison experience. One pathway travels down the autonomic hierarchy away from safety. The other maintains a ventral vagal state and an active Social Engagement System.
In a ventral vagal state, clients can savor the experience of regulation. They have an ongoing sense of connection and curiosity about others. In this active ventral vagal experience, neurobiology supports social connection, communication, and cooperation. The story is one of abundance.
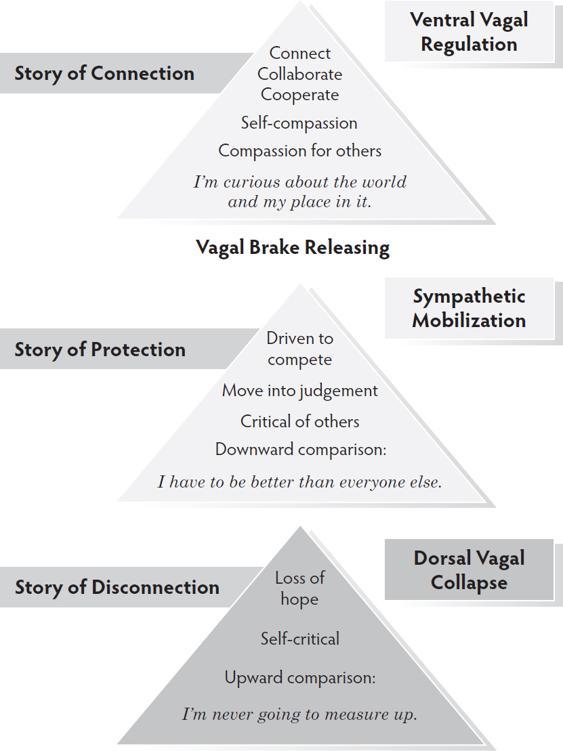
When clients move out of the regulation of ventral vagal, they move out of abundance into a mindset of scarcity.
In a state of sympathetic mobilization, clients move into a downward comparison where their survival depends on being better than everyone else. To move out of this fear, help your client first recognize the state and then discharge some energy safely. The vagal brake has to re-engage to move out of the story of protection.
In a state of dorsal vagal disconnection, clients move into an upward comparison and a belief that they can never compete with someone else. To begin the move out of this story of hopelessness and upward toward regulation, engage with your client in a small act of mobilization or help them remember a moment of safe connection.
The Experience of Comparing
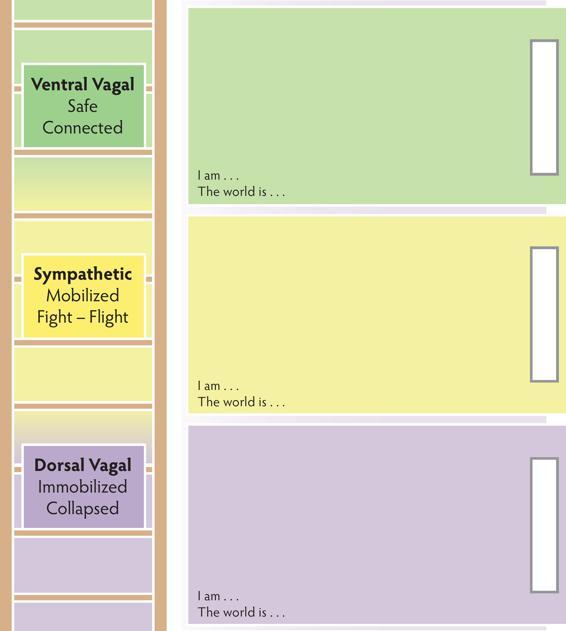
The Personal Profile map answers the question “Where am I?”
The Personal Profile Map helps clients identify their placement on the autonomic hierarchy. This map creates the basic skills necessary for recognizing autonomic states. With the Personal Profile Map, clients describe their somatic, thinking, feeling, and acting landmarks for each state.
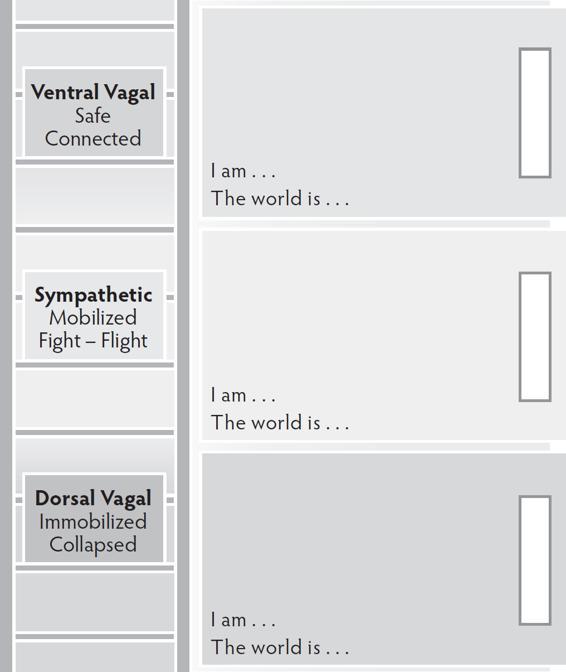
DIRECTIONS FOR COMPLETING
For each section, have your client choose a colored dry erase marker that represents the autonomic state. Ask your client to remember a time when they felt the sense of activation in that state. For sympathetic and dorsal vagal, invite just enough activation into mind and body awareness to get a flavor of the state. For ventral vagal bring the full experience into mind and body awareness and let the state come to life.
Map sympathetic and dorsal states first and end with mapping the ventral vagal state. (Whenever you are working with the autonomic hierarchy, the rule is to always end the process in ventral.)
As your clients map each section, have them fill in the corresponding space on the ladder describing body sensations, emotions, thoughts, and behaviors. What happens in their body? What do they do? What do they feel? What do they think and say? Ask how sleep, eating, and use of substances or addictive behaviors is impacted. After your clients complete each section, have them fill in the sentences “I am . . .” and “The world is . . .” These two sentences identify core beliefs at work in each state. The rectangles on the side of each section of the ladder are for your clients to label dorsal, sympathetic, and ventral in their own words.
Personal Profile Map
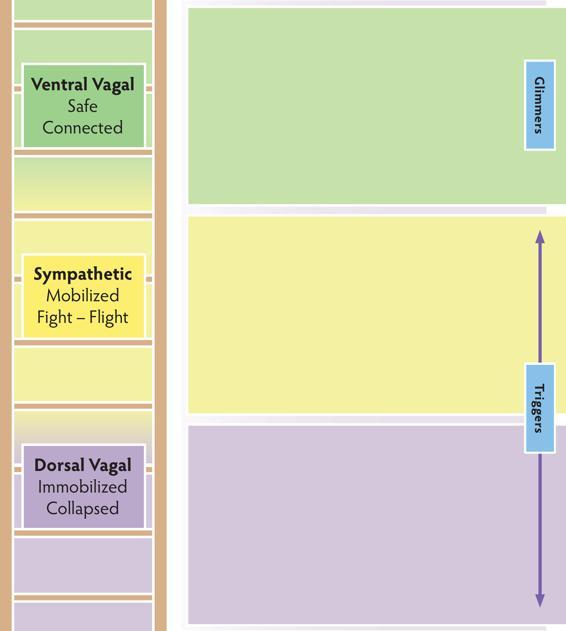
The Triggers and Glimmers map answers the question “How did I get here?”
The Triggers and Glimmers Map helps clients discover what activates their autonomic states by identifying what happens in their bodies, in the environment, and in relationships. Triggers are the cues of danger that energize sympathetic and dorsal vagal states while glimmers are the moments the ventral vagal system lights up. It is important to recognize both and not get caught in the loop of focusing on dysregulation.
When completing this map, clients need to be concrete in identifying specific triggers and glimmers. Specificity supports an ability to recognize, anticipate, and work with dysregulation and to replicate moments of regulation.
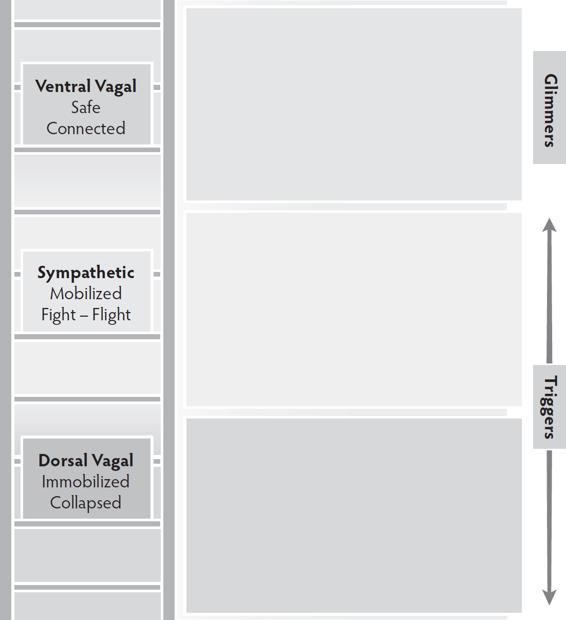
DIRECTIONS FOR COMPLETING
For each section, have your client choose a colored dry erase marker that represents the autonomic state. Triggers are what bring clients to therapy, and they are usually easily identified. Have your client begin with the survival response that is most familiar (sympathetic or dorsal vagal) and first map the triggers found in that state and then map the other. When the two “protection” sections are complete, end by mapping the glimmers of the ventral vagal “connection” section.
Triggers and Glimmers Map
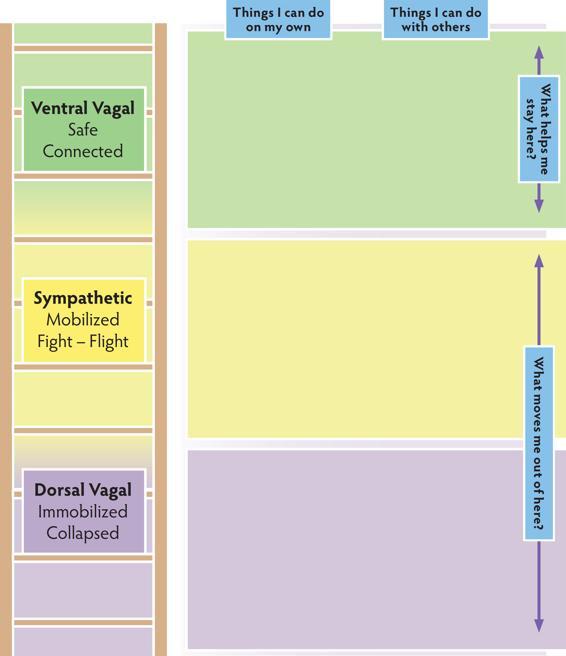
The Regulating Resources Map answers the question “How do I find my way back to ventral and stay there?”
The Regulating Resources Map helps clients identify actions in the two categories of self and co-regulation. This map brings attention to the presence and absence of individual and interactive resources, as well as the process of building new regulating pathways.
Utilizing resources tones the nervous system, activating the regulating pathways of the ventral vagal state, creating physical and psychological resilience.
This map targets identifying resources already present, creating resources where they are absent, and bringing balance to individual and interactive resources.
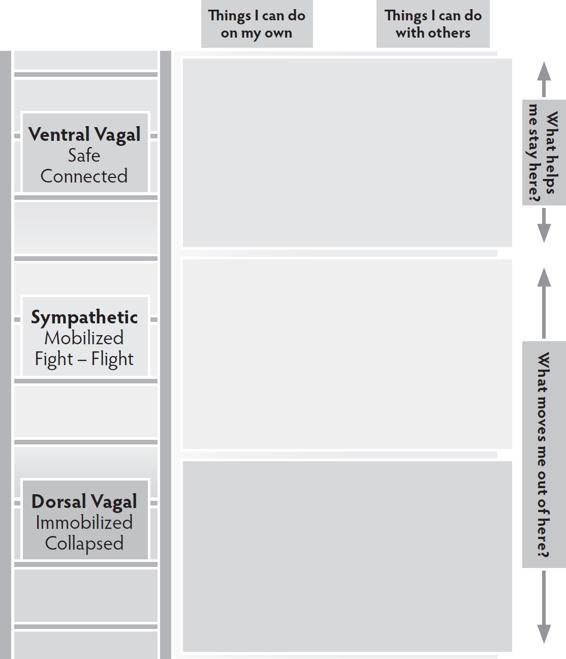
DIRECTIONS FOR COMPLETING
Have your client choose two colored dry erase markers—one for the left and one for the right side of the map. This creates a clear picture of balance and imbalance between the two regulating categories. Begin with the survival state that is most familiar to your client (sympathetic or dorsal vagal) and map both individual and interactive resources for that state. Then move to mapping the other survival state. End by mapping the ventral vagal state.
Regulating Resources Map
This version of the ladder map is suitable for working with kids.
The Time and Tone map can be used to track the flow of a session and also to map a specific experience. Use the horizontal axis to mark the time and the vertical axis to mark the state.
To map a session, have your client identify their beginning state, stop several times during the work of the session to mark where they are on the ladder, and again at the end of the session. Connect all the marks to see the autonomic path of the session.
To map an experience, listen with your client as they tell the story of an event. Mark the beginning state, stop to mark the state multiple times as the story unfolds, and then mark the state at the end. Connect the marks to see the autonomic story of the experience.
Note to Readers: Standards of clinical practice and protocol change over time, and no technique or recommendation is guaranteed to be safe or effective in all circumstances. This volume is intended as a general information resource for professionals practicing in the field of psychotherapy and mental health; it is not a substitute for appropriate training, peer review, and/or clinical supervision. Neither the publisher nor the author(s) can guarantee the complete accuracy, efficacy, or appropriateness of any particular recommendation in every respect.
Copyright © 2020 by Deborah A. Dana
All rights reserved
First Edition
For information about permission to reproduce selections from this resource, write to Permissions, W. W. Norton & Company, Inc., 500 Fifth Avenue, New York, NY 10110
For information about special discounts for bulk purchases, please contact W. W. Norton Special Sales at specialsales@wwnorton.com or 800-233-4830
Cover and interior design by Anna Reich
Interior composition by Vicki Fischman
Illustrator: Eric Hirsch, Graphic World
Illustration of Social Engagement System © Kate White,
Center for Prenatal and Perinatal Programs, ppncenter.com
Production manager: Katelyn MacKenzie
For more information on The Norton Series on Interpersonal Neurobiology, go to https://wwnorton.com/ipnbseries.
ISBN: 978-1-324-02009-7
ISBN: 978-0-393-71472-7 (ebk.)
W. W. Norton & Company, Inc., 500 Fifth Avenue, New York, N.Y. 10110
W. W. Norton & Company Ltd., 15 Carlisle Street, London W1D 3BS
Stephen Porges, Ph.D., is the creator of the Polyvagal Theory. Dr. Porges’s development of Polyvagal Theory offers a way to understand the neurophysiological systems that guide our daily living and has greatly influenced the practice of psychotherapy.
References:
Porges, S. W. (1995). Orienting in a defensive world: Mammalian modifications of our evolutionary heritage. A Polyvagal Theory. Psychophysiology, 32(4), 301–318.
Porges, S. W. (1998). Love: An emergent property of the mammalian autonomic nervous system. Psychoneuroendocrinology, 23(8), 837–861. https://doi.org/10.1016/S0306-4530(98)00057-2
Porges, S. W. (2001). The polyvagal theory: phylogenetic substrates of a social nervous system. International Journal of Psychophysiology, 42(2), 123–146.
Porges, S. W. (2003). Social engagement and attachment: A phylogenetic perspective. Annals of the New York Academy of Sciences, 1008(1), 31–47.
Porges, S. W. (2004). Neuroception: A subconscious system for detecting threats and safety. Zero to Three (J), 24(5), 19–24.
Porges, S. W. (2007). The polyvagal perspective. Biological Psychology, 74(2), 116–143. https://doi.org/10.1016/j.biopsycho.2006.06.009
Porges, S. W. (2011). The polyvagal theory: Neurophysiological foundation of emotions, attachment, communication, self-regulation. New York: Norton.
Porges, S. W. (2017). The pocket guide to the polyvagal theory: The transformative power of feeling safe. New York: Norton.
Porges, S. W., Doussard-Roosevelt, J. A., Portales, A. L., & Greenspan, S. I. (1996). Infant regulation of the vagal “brake” predicts child behavior problems: A psychobiological model of social behavior. Developmental Psychobiology, 29(8), 697–712.
Porges, S. W., & Dana, D. A. (2018). Clinical applications of the polyvagal theory: The emergence of polyvagal-informed therapies. New York: Norton.